A very simple question is changing the delivery of medical care: How is your health affecting your quality of life?
For decades, numbers drove the treatment of diseases like asthma, heart disease, diabetes, and arthritis. Public-health officials focused on reducing mortality rates and hitting targets like blood-sugar levels for people with diabetes or cholesterol levels for those with heart disease.
Doctors, of course, are still monitoring such numbers. But now health-care providers are also adding a whole different, more subjective measure—how people feel about their condition and overall well-being. They’re pushing for programs where nurses or trained counselors meet with people and ask personal questions like: Is your condition inhibiting your life? Is it making you less happy? Does it make it hard to cope day to day? Then the counselors offer advice about managing those problems and follow up regularly.
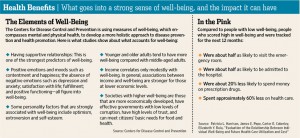
The logic is simple. People are more likely to manage their condition properly when they have more accessible, personal goals, like being able to do more at work or keep up with their kids, instead of focusing only on comparatively abstract targets like blood-sugar levels. And that, in turn, leads to much better health. Numerous studies show that when people have a higher sense of well-being, they have fewer hospitalizations and emergency-room visits, miss fewer days of work and use less medication. They’re also more productive at work and more engaged in the community.
“Quality of life happens to be the element that is most important in motivating people to deal with an illness,” says Noreen Clark, director of the Center for Managing Chronic Disease at the University of Michigan. “People aren’t motivated to follow their clinical regimen if in fact it doesn’t improve the way they function and get along with others and manage day to day.”
Breathing Easier
Focusing on well-being might seem like a basic idea, but it is a departure from the traditional approach to public health, especially when it comes to chronic-disease sufferers. Many get brief checkups with a doctor a few times a year, and there isn’t time for much beyond getting lab tests, a prescription and some directions to follow. And once patients leave the office, there is little that most doctors can do to make sure they stick to their regimen or help them with any problems or barriers to staying on the wagon.
For an idea of how the new emphasis works, consider Quentonia Ford. Struggling with severe asthma for 25 years, she found it hard to fully understand and manage her medications after brief doctor visits. Often gasping for breath, she had to curtail activities with her husband and family, and sometimes her symptoms got so bad she was hospitalized.
 Last year, she took part in Women Breathe Free, a program under study at Dr. Clark’s center at the University of Michigan that aims to improve the well-being of African-American women with asthma.
Last year, she took part in Women Breathe Free, a program under study at Dr. Clark’s center at the University of Michigan that aims to improve the well-being of African-American women with asthma.
“They asked about my quality of life, my family support, whether asthma stopped me from going out and doing the things I liked to do, even how it affected my sex life,” says Ms. Ford, 63 years old, who works as an administrative assistant for a hospice program. “No doctor ever asked me questions like that before.”
Ms. Ford says the program’s counselors, whom she spoke to over several weeks by phone, provided “a sounding board” about many concerns that were bothering her, and helped her understand her medications and how to use them more effectively. In the past, she would wait until her symptoms were severe, hoping things would get better; she now monitors herself more closely by keeping a diary of symptoms and using a device that monitors breathing to let her know if she is entering a danger zone.
Talking to a counselor regularly also helped her overcome fear and depression about her condition, and set reasonable goals for exercise and activity without fearing an asthma attack. In addition, she got the resolve to talk to her family about helping out more with things around the house and recognizing that she couldn’t do everything they wanted. She has not been hospitalized since she started the program, and last month her doctor told her that her pulmonary-function tests were the best she has had since 2006. She credits the counseling for giving her the tools and is continuing to provide information to the program so they can monitor her progress. “I never had anyone to talk to who understood me or what I was dealing with,” Ms. Ford says. “It has really helped me have more self-confidence and a better outlook about my quality of life.”
Measuring Results
Programs like Women Breathe Free are gaining traction as chronic illness eats up 75% of the $2.6 trillion the U.S. now spends annually on health care—and evidence mounts about the importance of quality of life.
In a study used to develop Women Breathe Free, for instance, nurse health educators provided regular telephone counseling for patients, talking to them about their particular asthma concerns, such as problems related to household cleaning or laundry products, and the use of birth-control pills or hormone-replacement therapy, which can exacerbate symptoms. Compared with a group that didn’t get the program, after two years the participants reported higher levels of asthma-related quality of life and a greater reduction in the use of certain medications. They also had a decrease of asthma symptoms with sexual activity and a greater reduction in missed days of school and work.
In the February issue of Population Health Management, a study found that higher self-reported well-being was associated with fewer hospitalizations, ER visits and medication use—and concluded that efforts to improve well-being are a promising approach to reduce future health-care use and spending.
Results like these have caught the attention of policy makers. The 2010 Affordable Care Act included $3 billion in funding for a new Patient-Centered Outcomes Research Institute, which will use quality-of-life measures as part of its evaluation of new treatments. And in a report issued in January, the Institute of Medicine, an independent group that advises the government on health policy, called for a new national action plan to identify programs that help those with chronic illness and the population as a whole “live well”—reflecting “the best achievable state of health that encompasses all dimensions of physical, mental and social well-being.”
The Institute of Medicine’s report “really pushed us into thinking about how health-related quality of life can be used to evaluate our program activities, in addition to looking at measures of mortality and the delivery of clinical services,” says Wayne Giles, director of the division of adult and community health at the Center for Chronic Disease Prevention and Health Promotion, part of the Centers for Disease Control and Prevention. “If there are things we can do to reduce pain and increase function, we may help delay the proportion of people who need nursing-home care and see reductions in hospitalizations and medical visits.” He adds: “And those are huge drivers of costs.”
Growing Effort
To measure health-related quality of life, the CDC queries more than 430,000 people each year through itsBehavioral Risk Factor Surveillance System, which measures the number of “healthy days” people have in a given month. Nationally, the trend isn’t good: Newly released data show the number of physically unhealthy days has barely budged over a decade, rising slightly to 3.6 days in 2009 from 3.3 days in 2000. The number of people who reported 14 or more mentally unhealthy days rose to 10.6% of the population from 9.6% over the same period. Rosemarie Kobau, a public-health adviser on quality-of-life programs at the CDC, says the measures will be instrumental in reducing health disparities, identifying unmet needs and tracking progress toward the federal Healthy People 2020, goals set by the federal government to improve the health of Americans over the next decade.
“Well-being moves us closer to looking at health in a positive sense—as more than the absence of illness,” Ms. Kobau says.
The measures are already being used to evaluate programs for care of those with widely prevalent diseases like arthritis, the most common cause of disability. Terry Brady, head of the CDC’s arthritis program, says the Healthy Days measures helped when the agency decided to scale back its funding to 12 states from 36 in 2008, providing larger individual grants to fewer states. The states that continued to receive funding were those with the highest success in linking patients to community-based programs that helped them manage their own disease and improve function, pain and quality of life.
Measuring quality of life and well-being is also helping states and communities identify vulnerable populations and design interventions to help. A program sponsored by the Robert Wood Johnson Foundation, Mobilizing Action Toward Community Health, has been using such data to rank the health of counties around the U.S.
As rankings have been released publicly over the past few years, says Patrick Remington, co-director of the program and associate dean for public health at the University of Wisconsin School of Medicine and Public Health, media coverage of poor rankings “has gotten people to think about the health of their community not just by whether it has a high death rate or short life expectancy but maybe a place where the quality of life is not as good as it could be.”
In 2006, Juneau County, Wis., was ranked as the unhealthiest community in the state—the lowest of 72—which county health officer Barb Theis says was a wake-up call. With a fairly rural population just under 28,000, nearly 30% of pregnant women smoked cigarettes, the teen birthrate was high, and nearly 40% of country residents hadn’t visited a dentist in the past year.
Ms. Theis got help securing funding for women and children’s services including a prenatal-care-coordination program and a dental clinic; she is now pushing for a mental-health clinic as well. In the 2011 survey, the county rank had risen to 52. “None of this would have happened without the rankings, because everybody here is taking ownership of improving the quality of life and health of our population,” she says.
This article was originally published in the April 16, 2012 edition of The Wall Street Journal.